

针对在线学习版块做简单的介绍,文字信息长度不可超过两行
A fully functional, independent woman who is nearly 100 years old lives with her 2 daughters. A history finds that she has:
Her medications are lisinopril, furosemide, ASA, and metoprolol.
Patient develops abdominal pain increasing over 5 days; obstipation for 1 day. She is acutely ill and she appeared uncomfortable and volume depleted. On exam, she has abdominal distention, hypoactive bowel sound and no mass is found. Her heart is enlarged and no S3.
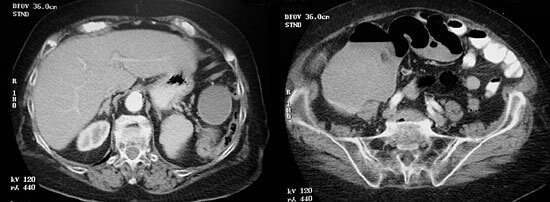
An abdominal CT scan (shown below) shows the cecum is very dilated to 13cm and the left image show a possible mass in the descending colon.
Recognizing the seriousness of her illness she was quickly stabilized with volume repletion. She was in the emergency department two hours then admitted to a non-intensive care surgical unit. And cared for by a general surgeon and a geriatrician.
Protocol calls for endoscopy, but to do so would require a delay before surgery that is clearly needed. There was an urgency to get her to surgery as delays would likely lead to complications. Accordingly, no colonoscopy was performed. Prior to surgery, careful anesthesia planning and intra-operative management was designed. A shortened bowel prep was initiated.
A left hemicolectomy was performed on day 2. Pain was controlled with low doses of morphine and fluid management was tightly managed. She was provided a single, quiet room and a family member stayed with her continuously.
The patient was discharged to subacute rehabilitation on day 5, and then to home on day 10.
Post-operative complications are very common, especially in very old patients and their occurrence can be devastating. Minimizing the chance of such complications is critical in order to avoid a deteriorating cascade of iatrogenic events. Potential common post-operative complications and how they were avoided in this patient are listed in the table below.
| Problems | Prevention Strategies |
|---|---|
| Prolonged delirium | Daughter slept in the room and patient was not in intensive care |
| UTI | Catheter was removed one day post-op |
| Pneumonia | Spriometry and quickly she was gotten out of bed |
| Volume depletion/fluid retention | Careful examinations and frequent adjustments in orders |
| Fall | The daughter remained in the room with the patient |
| Pressure sores | Turning and skin care was done 3x/day |
| GI bleed | PPI |
| DVT/PE | Prophylaxis with anticoagulants |
The very old tolerate major surgical operations but they are not able to tolerate post-operative complications. More patients such as this one will be prominent in medicine in the future as the over 85 years of age segment of the population is the fastest growing portion of the U.S. population. The elderly are more vulnerable with multiple co-morbidities and minimal physiologic reserves. Geriatric surgery, like pediatric surgery 60-70 years ago, is a developing discipline today. Listed below, Dr. Katlic* outlines six principals underpinning the movement in geriatric surgery.
I. Presentation
-Subtle/atypical/delirium
II. Lack of Reserve
-Especially after age 80, extreme after 90
III. Preoperative Preparation
-Must be ideal because of above and multiple chronic diseases
IV. Emergency surgery
-Risk increases 3-10x fold morbidity and mortality; LOS is prolonged
V. Attention to detail
-“Elderly tolerate operations but not complications”, anonymous
VI. Age a fact
-Avoid agism: a pervasive problem
*Katlic, M. Principles of Geriatric Surgery in Principles & Practice of Geriatric Surgery. Eds: Rosenthal RA, Zenilman ME, Katlic MR. Springer, New York, 2001.
The has been a paradigm shift in health care over the past century that will continue over the next 50 years with the increasing numbers of elderly patients. The elderly are more vulnerable patients because they havemuch less homeostatic reserve than when they were younger, and typically they have multiple chronic health problems complicating their acute illnesses and management.
(data sources: U.S. Census Bureau & National Center of Health Statistics)
At the turn of the last century, we in the U.S. had many young in proportion to only a few old individuals. By the year 2000, that changed and the proportion of old to young is much greater. Furthermore, the baby boomers (those born from 1945-1960) as they become elderly will dominate the health care system.
The curves in the graph to the right show the remarkable growth and the anticipated growth of the elderly population in the U.S. The population of those over 85 years is the most rapidly growing segment of our society.
Graphed below are theoretical representative curves of physiological function (y-axis) showing changes associated with normal aging (x-axis). These were simplified from the data of the Baltimore Longtudinal Study of Aging, NIA, NIH.
Loss of homeostasis resulting in less reserve to withstand perturbations is a major issue in older patients and must be considered in caring for elders who are ill. Older patients are medically typically more complicated than the middle aged because of the presence of multiple health issues, such as those common problems listed below:
This results in the elderly disproportionately using the health care system. While the elderly currently make up about 14% of the population, they account for a much larger percentage of health care usage. Warshaw and Bragg (Part of ADGAP Longitudinal Study of Training and Practice in Geriatric Medicine, Jan. 2004) found in 2000 that the elderly accounted for 55% of all ambulatory care visits to specialists, up from 40% in 1980.
Currently the elderly use the health care system disproportionately to their presence in the population. The elderly still only account for about 14% of the population but account for nearly 45% of hospitalizations. The demographic imparative which now is upon us will cause the elderly to dominate the health care system including the requirement for surgery. American medicine is not yet prepared for this but must be in the next decade. Advances in geriatric surgery must be a major part of this preparedness.